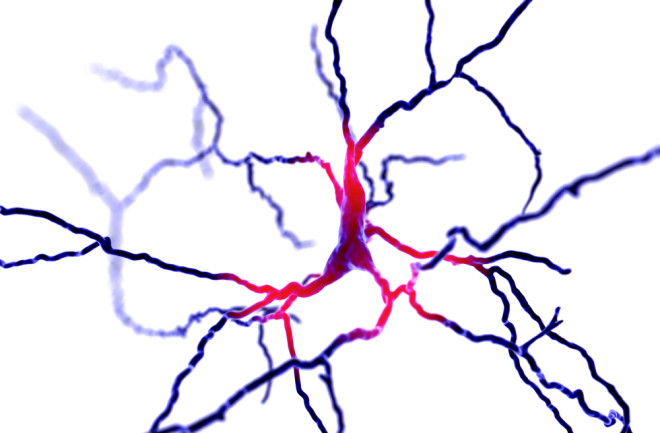
In the field of neuroscience, a recent study claims to have finally unravelled a longstanding mystery – how do the cells of individuals with Huntington’s disease produce detrimental amyloid proteins from other proteins, resembling a game of destructive Lego? These amyloids gather in nerve cells, forming plaques that ultimately lead to cell death and contribute to the progressive symptoms associated with Huntington’s. The investigation was conducted by Randal Halfmann and his team at the Stowers Institute for Medical Research, a non-profit biomedical research organization. To examine the protein Lego, the researchers employed a new technique called Distributed Amphifluoric Förster Resonance Energy Transfer (DAmFRET) to observe real-time changes in individual cells. After careful analysis, they were able to provide a surprisingly uncomplicated explanation for the origin of amyloids.
The genetic mutation responsible for Huntington’s Disease has been relatively well-understood thus far. Individuals with the disease have a mutation in their genes that encode for a protein called Huntington, which contains an excessive amount of the amino acid glutamine. Glutamine serves as a common building block for proteins. To develop Huntington’s, one must possess at least 36 consecutive glutamine residues, with more repetitions resulting in more rapid symptom progression. This segment of repeated glutamine, known as the polyglutamine or “polyQ” segment, is linked to nine different fatal diseases, with Huntington’s being the most prevalent among them. Remarkably, the polyQ segment renders the huntingtin protein more prone to aggregation, making it more likely to form amyloids. These amyloid proteins are composed of layered sheets that originate from a complex mechanism commonly referred to as an “amyloid nucleus.”
Despite the long-standing curiosity surrounding the amyloid nucleus, its identification has remained elusive due to its transient, rare, and unstable nature. A 2021 preprint paper states that even computer simulations are inadequate due to the uncommon structure and the involvement of numerous variables. However, using the DAmFRET technique with a “direct intracellular reporter,” the researchers determined that the nucleus was astonishingly simple – a minuscule structure consisting of four strands found within a single protein molecule. Once formed, this nucleus triggers the formation of amyloid fibers, which accumulate to form plaques. Halfmann emphasizes that this discovery suggests a major paradigm shift, where everything stems from a single event – a spontaneous alteration in protein shape. This event sets off a cascade of amyloid formation, leading to cellular death and potentially providing crucial insights into the disease-causing mechanism of amyloids.
The paper also sheds light on a potential medical strategy: polyQ molecules fail to form nuclei when crowded alongside other proteins. They require sufficient space to develop this structure, and a potential treatment might involve obstructing this process. Although there are various medications available to alleviate the symptoms of Huntington’s disease, none have the ability to halt or slow down the disease itself. Pridopidine, an investigational drug, aims to combat the condition by stimulating the release of a regenerating chemical in the brain. Furthermore, the DAmFRET findings could have wider implications in the field of neurodegenerative diseases, such as Alzheimer’s and Parkinson’s, where the accumulation of amyloids is also a contributing factor.
In conclusion, the recent breakthrough in understanding the origin and formation of amyloids in Huntington’s disease has provided valuable insights into the disease mechanism. This revelation opens up new possibilities for potential treatments and further research in related neurodegenerative disorders. The findings from the DAmFRET technique have the potential to revolutionize our understanding of these diseases and pave the way for novel therapeutic strategies.